With near-constant updates on the number of COVID-19 cases confirmed globally, you’ve probably heard about various methods to screen for the virus that causes the disease. Although several, well-proven methods already exist to detect the virus, laboratories around the world are experimenting with new tests and methods to provide faster and even more reliable screening. Despite these new developments, the “gold standard” of test methods for COVID-19 is the RT-PCR test.
Reverse transcription polymerase chain reaction (RT-PCR) is a reliable, highly sensitive method for detecting the SARS-CoV-2 virus, which causes the COVID-19 coronavirus disease. Although the test can be performed on bench-top instruments capable of analyzing one or a few samples at a time, most RT-PCR tests are conducted by large workstations capable of processing thousands of samples per day, located in hospitals, clinics, and specialized testing facilities.
Here’s an overview of how the RT-PCR test works:
A test sample (typically taken by a swab from the patient’s throat or nose) is treated with chemicals to remove fats and proteins so the virus’ RNA can be extracted. (Note that SARS-CoV-2 has only RNA, no DNA.) The RNA is then converted to DNA using a reverse transcriptase enzyme (this is the “RT” part of “RT-PCR”). This step is necessary because RNA cannot be amplified, or copied, but DNA can be. Short fragments of DNA (referred to as “primers”) that are complementary to the viral DNA are added. If viral DNA is present, these fragments attach to the target sections of the viral DNA. The mixture is then heated and cooled cyclically to trigger chemical reactions, using a type of enzyme known as a polymerase, to create copies of the target sections of the viral DNA. The copying of DNA sections is referred to as “amplification,” and there are typically 20 to 40 cycles, with each cycle doubling the previous amount of the target DNA. As copies of the target DNA are made, a fluorescent molecule (referred to as a “probe”) is activated, releasing fluorescent dye. When the level of fluorescence exceeds a baseline, or target amount, the presence of the virus is confirmed. The number of cycles, or amplifications, required for detection of the virus indicates the severity of the infection.
So the RT-PCR test method involves a relatively straightforward, but highly sensitive set of chemical and biological reactions…but what do linear motion and automation have to do with the process?
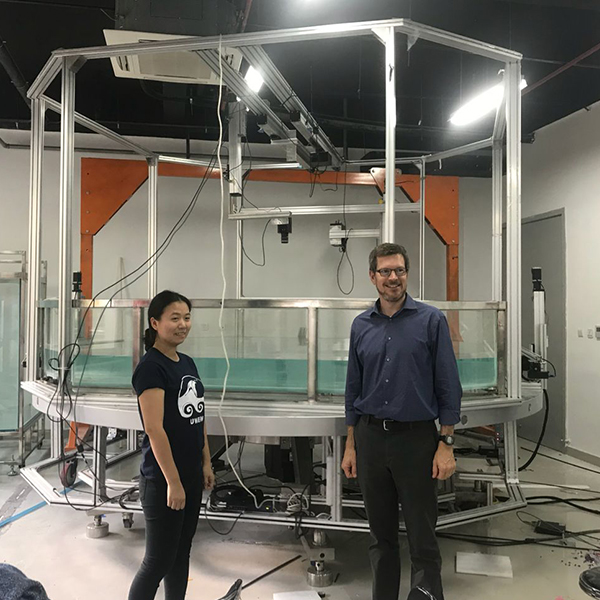
First, automation — and linear motion systems in particular — make it possible to carry out the shear volume of RT-PCR tests that are required during a global health emergency such as the SARS outbreak or the COVID-19 pandemic. Not only do samples and consumables need to be loaded, unloaded, and moved through the various steps of the process, liquid handling is also required at key stages of the test procedure.
Here are a few examples of how linear motion systems are used in RT-PCR testing:
Gantry robots with rotary end effectors remove caps from sample tubes. Liquid handling robots — typically small Cartesian or gantry systems — extract samples from and dispense liquid enzymes into sample tubes and plates. Linear actuators or belt conveyors move samples – individually or in trays – through the workstation for each step of the testing process. Linear actuators apply labels and barcodes to samples
Of course, all these tasks could be done by human workers, but linear actuators and robots can work faster and longer than humans. And they can work error-free, without misapplying labels or spilling critical samples or reagents.
When these functions are carried out by automated linear systems, the number of tests that can be performed per hour or per day is increased, the instance of errors is decreased, and the ability to track samples is improved. The safety of clinical and laboratory personnel is also improved, since contact with potential contagions is reduced.
All of this means that physicians, clinicians, and patients are provided with reliable test results in the shortest time possible.
Post time: Oct-24-2022